The Big Picture | What Is It? | Diagnosis | Understanding Risk | Treatment Options | Prostate Cancer Results Study Group
Results of Treatment Prostate Cancer Results Study Group (PCRSG)
There are currently no randomized studies comparing the effectiveness of modern treatments. A randomized study is one in which patients voluntarily undergo whatever treatment is chosen for them. Most patients want to choose their treatment. Therefore, we are limited to studies that look at a single treatment and then try to compare them. In an effort to compare these treatments from center to center, the following prostate experts (the Prostate Cancer Results Study Group or PCRSG) from around the world have cooperated to review the world’s literature. This is an ongoing effort and will be updated regularly here at the Prostate Cancer Center of Seattle. If you wish a updated version please contact Lisa at Lisa@pccseattle.com and request the PCRSG results. The Prostate Cancer Results Study Group comparative analysis study is supported by the Prostate Cancer Treatment Center Foundation.
Study Experts
- Peter Grimm, DO, Prostate Cancer Center of Seattl
- Ignace Billiet, MD, Europe
- David Bostwick, MD, Bostwick Laboratories
- David Crawford, MD, University of Colorado
- Brian Davis, MD Mayo CLinic Rochester , Minnestoa
- Addam Dicker, MD Thomas Jefferson U Philadelphia Pa
- Jos Immerzeel, De Prostaate Kliniek Netherlands
- Steven Frank, MD MD Anderson Houston Texas
- Mira Keyes, MD, BC Cancer Agency Vancouver , BC
- Patrick Kupelian,, MD, UCLA
- Stephen Langley, MD St Luke’s cancer centre, Guildford, England
- Robert Lee, Duke University Medical Center
- Stefan Machtens, MD, Europe
- Alvaro Martinez ND. Michigaan
- Brian Moran, MD, Chicago Prostate Center
- Greg Merrick, MD, Schiffler Cancer Center
- Jeremy Millar, MD, Australia
- Luis Campos-Pinheiro, MD, New University of Lisbon
- Mack Roach, MD, UCSF
- Richard Stock, MD, Mt. Sinai, New York
- Katsuto Shinohara, MD, UCSF
- Mark Scholz, MD, Prostate Cancer Research Institute Marina Del Ray California
- Ed Weber, MD, Prostate Cancer Center of Seattle
- Anthony Zietman, MD, Harvard Joint Center
- Michael Zelefsky, MD, Memorial Sloan Kettering, Fellows
- Jason Wong, MD UC Irviene California
- Jyoti Mayadev, MD UC Davis California
- Robyn Vera, DO, Radiant Care Olympia , Washington
Purpose of the PCRSG
The purpose of the PCRSG is to compare and share results for prostate cancer that are understandable to both patients and physicians. The study group, to date, has reviewed greater than 25,000 articles published from 2000-2012. These articles have come from all available respected journals. From these articles, 1066 Treatment Results Articles were identified as related to treatment. The expert panel agreed that many studies were poorly done and therefore established the following criteria for inclusion of an article to allow comparison of different treatments. If you wish a updated version please contact Lisa at Lisa@pccseattle.com
Criteria for An Article to Be Included for Comparison Purposes
- Patients must be stratified into recognizable Pre-Treatment Risk Groups: Low, Intermediate, and High Risk by either D’Amico, Zelefsky or NCCN stratification. The risk group must be maintained after treatment.
- A biochemical (PSA) result must be reported by standard means recognizable and comparable. BRFS (biochemical relapse free survival)* standard endpoint ASTRO, Phoenix, and PSA < 0.2 (surgery).
- Patients must be clinically staged pre-treatment. Stage**
- No exclusions. I.e. No Pathologic staging. In other words after surgery the surgeon could not eliminate or exclude a patient from future analysis because of an unfavorable feature (positive margin, positive lymph nodes)
- External doses must be modern doses. Minimum 72 Gy*** IMRT/conformal.
- All treatment modalities must be considered; Seeds, Surgery, IMRT, HIFU, CRYO Protons and/or HDR.
- Peer reviewed journals only. Peer reviewed journals are those in which every article is first reviewed by an expert panel before publication.
- Low Risk Accepted minimum number 100 pts. This is to insure an adequate number are evaluated.
- Intermediate Risk Accepted minimum number 100 pts.
- High Risk Accepted minimum number 50 pts.
- Minimum median follow up: 5 yr. This was to insure that patients were followed long enough to adequately evaluate the results long term.
How to Use These Results
Establish your risk group with your doctor. Look at the slides related to your risk group. The other risk groups will not be pertinent to your evaluation.
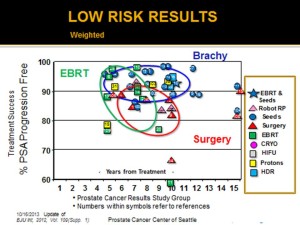
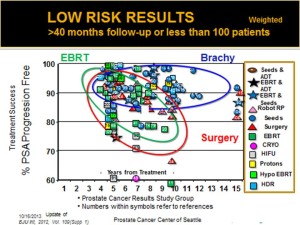
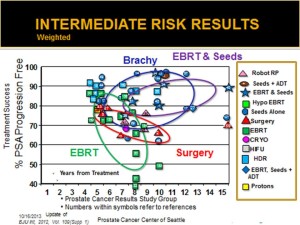
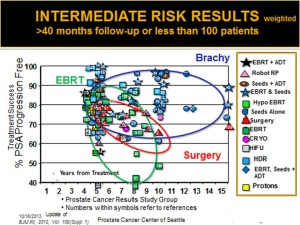
Each treatment is represented on the graph by a symbol. For example, the surgery results are represented by a red triangle and the seed implant (Brachy) alone is represented by a blue dot. The numbers within the symbol represents the article which can be found beneath the slide in the notes section.
The first slide in your risk group represents all of the articles that met the PCRSG criteria, the second includes a graphic that circles all the articles of that treatment and makes the comparison of results easier. The third and fourth slides look at results if the criteria are relaxed a bit to allow more studies for comparison. In all situations, the results do not substantially change when the criteria are relaxed.
Low Risk
Overall, 80% of all Low Risk patients will do well with any treatment. While it appears on the graphs that Brachytherapy does the best overall, it is apparent that most patients can do well with any treatment. Therefore, for cancer control purposes, we advise most patients that they cannot make a bad decision. However, there is a slight difference in results. Why does Brachytherapy appear to do slightly better overall than external beam or surgery? The difference may lie in the nature and capabilities of each treatment to address all of the cancer. If you wish a copy of the entire update version please contact Lisa at Lisa@pccseattle.com and request the PCRSG results. (Click on Graphs to enlarge)
The primary reason surgery fails in Low Risk prostate cancer is likely that disease around the nerve is left behind, which the pathologist can recognize post operatively or suspected when the PSA rises after surgery. Despite some statements by surgeons, it is not possible to see this microscopic disease at the time of surgery and make a decision at the time of surgery on whether to take the nerve. From the figures, it is apparent that, with low risk disease, the surgeon will leave cancer behind 15-20% of the time and, therefore, you will likely need post operative radiation, 15-20% of the time. Note, on the graphs, that there are no reported results yet for robotic surgery that met the criteria. However, results to date for robotic surgery have not shown any improvement in cancer control over standard radical prostatectomy. So these results are not expected to change.Surgery (Red Triangles)
Whether the surgery is an open radical or robotic radical prostatectomy, almost all surgeries done for low risk disease are nerve sparing. The risk of disease outside the gland with low risk disease, as predicted by the Partin Tables, ranges from 6-28%. The majority of this is disease that penetrates beyond the edge of the capsule called capsular penetration or sometimes extraprostatic extension. You can determine your risk of lymph node, capsular penetration and seminal vesicle involvement from the Partin Tables.
External Radiation (Green Squares)
There are several forms of this. IMRT (Intensity Modulated Radiation Therapy), Protons, Tomotherapy and Cyberknife. IMRT is the most common, with only a few long term studies for the other treatments. Patients should be aware that just because a therapy is new does not make it better. All of the external beam treatments give very similar biological doses (75-81 Gy) and, therefore, the results are also similar. The area treated is also similar. This area includes the prostate and a small margin. As can be seen in the graphs, external beam treatments do well for approximately 80% of the patients. Many years of study will still be required to ultimately determine whether any type of external beam treatment will actually be better.
External radiation does a good job of treating the prostate and the area immediately around it, where cancer can spread. The reason the external radiation fails in some low risk disease is likely that the dose delivered is not sufficient enough to control the disease in the prostate itself. The external dose that can be given to the prostate by external beam techniques is limited by the structures surrounding the prostate, primarily the rectum, bladder and hips. While techniques have been developed to minimize these areas receiving high doses, it is difficult to give doses beyond 75-81 Gy equivalent doses without a higher risk of rectal, bladder and hip injury.
Seed Implantation Alone/Brachytherapy (Blue Dots)
Brachytherapy has a very low local failure rate in the Low Risk setting. Local failure is reported to be less than 1% in reported series. The reason for this is that the dose delivered to the gland and tumor is considerably higher than external beam techniques. The dose with seeds are 120-145 Gy compared to 75-81 Gy for external beam. The reason seeds can deliver a higher dose to the cancer is that the seeds are placed directly into the gland and tumor. The dose from the seed falls off rapidly, resulting in lower doses to the bladder, rectum and hips than external radiation. Typical seed implant techniques also include the area where the cancer spreads and the planning for an implant always includes the area around the nerve. Reports on cancer spread beyond the gland have shown that disease is less than 3 mm from the gland in 98% of these low risk situations. By including a typical margin of 5-10 mm, the extraprostatic disease is covered by the doses from seeds. Therefore, seed implantation may do slightly better overall than surgery or external beam because it gives more dose to control the cancer in the prostate than external beam radiation and does better than surgery, which has excellent local control, and because seed implantation is designed to control the disease beyond the gland.
External Beam Radiation and Seed Implantation (Blue Stars)
A number of studies have included the addition of external beam radiation (EBRT) to seed implantation for Low Risk disease. The addition of external beam radiation is controversial and typically only recommended for low risk patients with a large number positive biopsies. The rationale for the external beam radiation in this setting is to cover disease that may have spread beyond the implant margin. Most patients will not need this additional treatment. If EBRT is recommended, it is generally because of a large number of positive biopsies or for technical reasons to cover areas not possible by an implant. The cancer control results are similar to implant alone and excellent for this approach. If you wish a copy of the entire update version please contact Lisa at Lisa@pccseattle.com and request the PCRSG results.
Intermediate Risk
Intermediate Risk disease is highly variable group of patients in terms of results and approaches. There is a wide variability of risk of disease beyond the gland ranging from 16-57% which can explain why the results vary widely. Also, the definitions are slightly different between centers, which makes comparisons more difficult.
The first step, once it has been determined that you fit in this category, is to determine what the risk of disease is beyond the gland. The Partin Tables can help determine for you, individually, what the risk might be. The good news is that, for many patients, intermediate risk disease behaves very similar to low risk disease and can be treated in a similar fashion. However, we help each patient determine what the risk of disease is beyond the gland and individualize the treatment to treat all of the disease both inside and outside the gland.
On first glance at the graphs, it appears that brachytherapy approaches with either permanent seed or HDR implants are superior to the either surgery or external beam radiation. There are no long term (> 5yrs) HDR studies to date, however. Why might there be an advantage to brachytherapy approaches? For intermediate risk patients, the risk of disease beyond the gland increases, subsequently, any treatment that just treats the prostate, such as surgery, has a higher risk of failing.
Surgery for Intermediate Risk (Red Triangles)
Surgery can be a good option, in this group, if the disease beyond the gland is calculated to be low. Many patients in this category can have surgery. Surgery likely fails in intermediate risk disease because there is a significant amount of disease beyond the prostate which the surgery doesn’t treat. The calculation of disease beyond the gland using the Partin Tables can be very helpful. If the risk of disease beyond the gland is low, surgery may be a very good option. The surgical results on the graphs likely represent a failure to carefully select patients who may be good candidates.
External Radiation Beam Therapy (EBRT) for Intermediate Risk Disease (Green Squares)
Because intermediate risk patients are at higher risk for disease beyond the gland, External Radiation for intermediate risk disease has the advantage over surgery of treating both the prostate and a wider area of potential spread. Conformal, IMRT (Intensity Modulated Radiation Therapy), Protons, Tomotherapy and Cyberknife are all forms of external beam radiation. Each has its own technical advantages. Conformal and IMRT are the most common forms, with the most results, with only a few long term studies for the other treatments. Patients should be aware that just because a therapy is new does not make it better. All of the external beam treatments give very similar biological doses (75-81 Gy equivalent) to the prostate and, therefore, the results are also similar. The area treated beyond the gland, which may include the seminal vesicles and lymph nodes, is also similar. As can be seen in the graphs, external beam treatments do well for approximately 60-80% of the patients.
External radiation does a good job of treating the prostate and the area immediately around it where cancer can spread. For intermediate patients, external radiation likely fails in this setting due to an inability to give enough dose to control the disease in the prostate itself. The external dose that can be given to the prostate, by external beam techniques, is limited by the structures surrounding the prostate, primarily the rectum, bladder and hips. While techniques have been developed to minimize these areas receiving high doses, it is difficult to give doses beyond 75-81 Gy equivalent doses without a higher risk of rectal, bladder and hip injury.
Brachytherapy/Seed Implantation for Intermediate Risk Patients (Blue Dots)
Brachytherapy (Seed implantation alone) has a very low local failure rate in the Intermediate risk setting. Local failure is reported to be approximately 1.4% in reported series. The reason for this is that the dose delivered to the gland and tumor is considerably higher than external beam techniques. The dose with seeds are 120-145 Gy (dose equivalent) compared to 75-81 Gy for external beam. The reason seeds can deliver a higher dose to the cancer is that the seeds are placed directly into the gland and tumor. The dose from the seed falls off rapidly, resulting in lower doses to the bladder, rectum and hips than external radiation.
Many intermediate patients behave similarly to low risk patients and can be treated with seed implantation alone. The Partin Tables can help determine for you, individually, what the risk might be of disease beyond the gland and whether seed implantation alone is appropriate. Typical seed implant techniques also include the area where the cancer spreads and the planning for an implant always includes the area around the nerve where most of the extraprostatic disease is found.
Brachytherapy Alone vs External Beam and Seeds for Intermediate Risk Disease
The value of external beam radiation (EBRT) with seeds is its potential to treat a wider area than seeds alone. This estimate of need for external beam for seeds takes into account the Partin Table calculation of risk beyond the gland, the number of biopsies that are positive, the risk of seminal vesicle involvement and whether there is nerve invasion. Each of these factors may influence your doctor’s opinion on the value of EBRT. The data from the graphs do not allow for a clear distinction on which patients should get seeds alone versus combined EBRT and seeds. We, therefore, have conducted several surveys of experts to ask their opinion on what treatment they might give for each clinical situation they might encounter in this group. These opinions will be shared and discussed with you at the time of consultation to help decided on the most appropriate approach in your situation.
Implantation alone, or in combination with EBRT, do appear, on the graphs, to do better than either surgery or external beam radiation. Seed implantation is likely better than surgery in intermediate risk disease due to the high local control rate of seed implantation and its ability to treat an area beyond the capabilities of surgery. Since external beam and seed implantation techniques treat a similar volume beyond the prostate, seed implantation with or without external beam radiation is likely better than external beam radiation because of the substantially higher dose to the prostate. Therefore, seed implantation techniques may do slightly better overall than surgery or external beam because it gives more dose to control the cancer in the prostate than external beam radiation and does better than surgery, which has excellent local control, because it is designed to control the disease beyond the gland.
High Risk Disease
Patients with Gleason Scores 8-10, Stage T2c or a PSA greater than 20 or two intermediate factors, such as a PSA 10-20 and Gleason Score 7, are considered to have high risk disease. High risk simply means that there is a higher risk that disease is outside the prostate. Estimates of risk of disease beyond the prostate range from 23-88%. Most patients in this group have a risk of at least 50%, making them poor candidates for treatments that treat the prostate alone (i.e. surgery, seed implantation alone, EBRT to just the prostate). The graph results for surgery, for example, demonstrate that only 25-50% of patients will be successfully treated with surgery. There are no “good” high risk patients which can be definitively identified as being better candidates for local treatment alone. The graphs demonstrate that more aggressive treatments which combine treatments generally have better results.
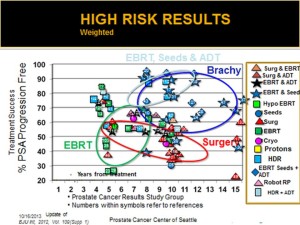
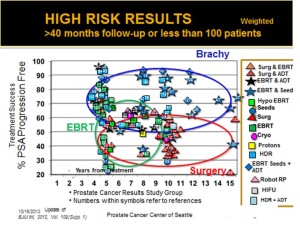
Surgery for High Risk Disease (Red Triangles)
Surgery is generally a poor option in this group because the risk of the disease beyond the gland is calculated to be high. Estimates of risk of disease beyond the prostate range from 23-88% with an average of at least 50%. Surgery likely fails in high risk disease because there is often a significant amount of disease beyond the prostate which the surgery cannot cover. If you have doubt about this, the calculation of disease beyond the gland using the Partin Tables can be very helpful to confirm this. We would rarely recommend surgery as a primary option for high risk disease.
External Beam Radiation (EBRT) for High Risk Disease (Green Squares)
The routine use of external beam radiation in this setting has as its rationale the ability of external beam radiation to treat microscopic areas beyond the prostate than either surgery or seeds alone cannot treat. EBRT alone in this setting has resulted in only 35-65% of the patients being successfully controlled. External radiation does a good job of treating the prostate and the area immediately around it where cancer can spread. For high patients, external radiation likely fails in this setting due to an inability to give enough dose to control the disease in the prostate itself. The external dose that can be given to the prostate by external beam techniques is limited by the structures surrounding the prostate, primarily the rectum, bladder and hips. While techniques have been developed to minimize these areas receiving high doses, it is difficult to give doses beyond 75-81 Gy equivalent doses without a higher risk of rectal, bladder and hip injury.
External Beam Radiation (EBRT) and Hormonal Therapy for High Risk Disease (Black Stars)
Hormonal therapy has been added to external beam radiation for high risk disease to try to improve the effectiveness of this modality. The rationale is to kill as many cancer cells prior to EBRT by temporarily blocking testosterone production. This approach thereby, theoretically, allows for fewer cells that the radiation needs to eradicate at the doses which can be safely delivered (75-81 Gy). For the most part, as demonstrated in the graphs, this can be accomplished. The results for this approach appear to be better than EBRT alone with 60-70% cancer control versus 35-65% with EBRT alone. The course of hormonal therapy is debated but most centers restrict the hormonal therapy to 6- 12 months with an occasional center giving it for up to three years.
External Beam, Seed Implantation Plus or Minus Hormonal Therapy for High Risk Disease (Blue Diamonds
The triple modality approach (External Beam, Seed Implantation and Hormonal Therapy) for High Risk disease begins with the rationale that Hormonal Therapy may reduce the number of cells that need to be killed. EBRT (IMRT) can deliver an adequate dose to kill microscopic disease beyond the gland and seed implantation can deliver a dose sufficient to control the disease within the gland. The small number of studies using this approach indicate that this rationale may be supported with cancer control rates long term of 85-92%. Note that this may be grade dependent as the subset of high risk patients with very high grade (9-10) in less mature studies usually fair worse. The use of external beam plus seeds appears to be quite variable from center to center. More studies will be needed to determine the best treatment. However, we have chosen, for high risk disease, to recommend a combination of six months of hormonal therapy during which both external beam and seed implantation are given. If you wish a copy of the entire update version please contact Lisa at Lisa@pccseattle.com and request the PCRSG results.